Food Allergy & Anaphylaxis
Treatment of Anaphylaxis
Allergy & Anaphylaxis Emergency Plans are designed to provide clear, concise instructions on how to quickly assess and manage symptoms of a developing allergic reaction. Symptoms may be mild at the beginning, but if left untreated may progress to more severe symptoms. This is why prompt treatment is essential, and is the main reason for why your doctor urges you to be very familiar with your allergy action care plan.
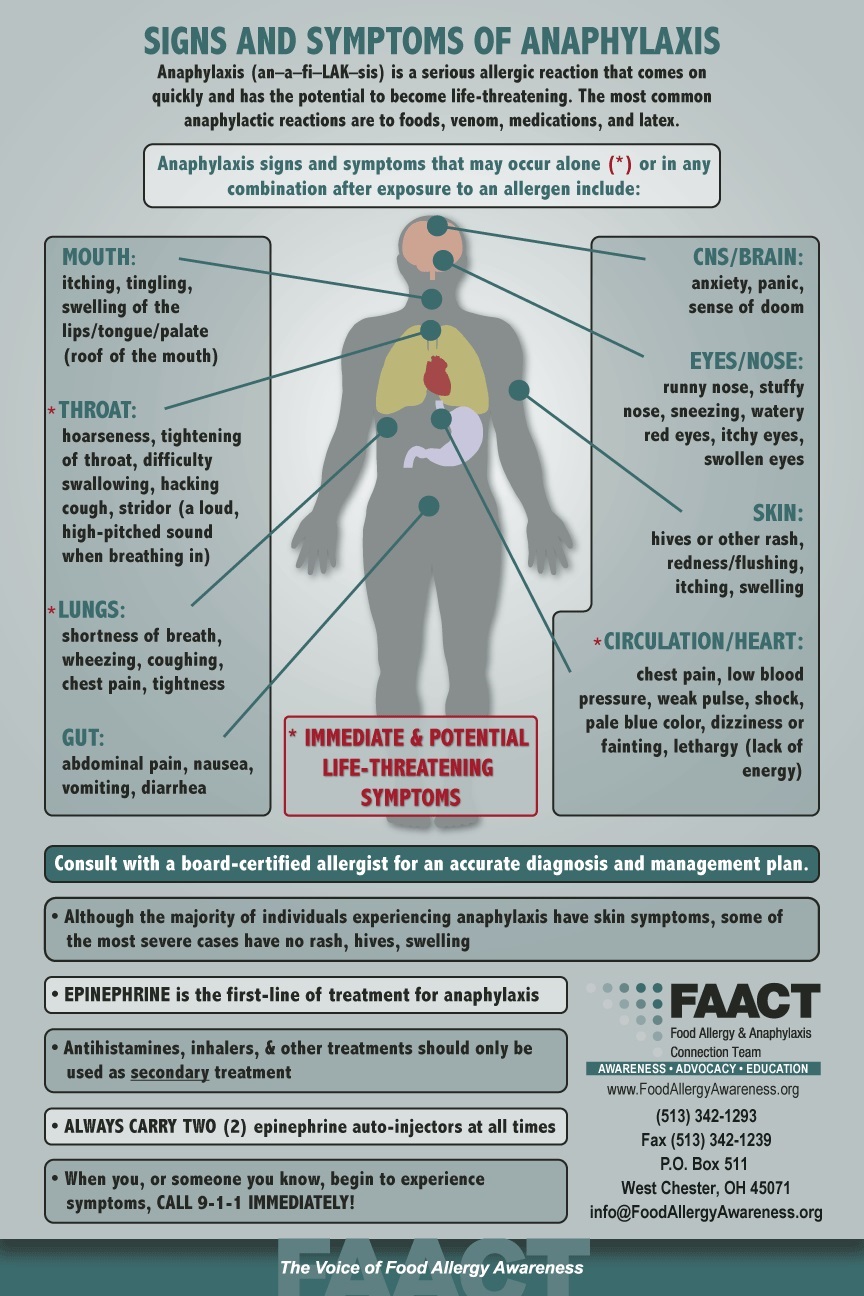
Treatment of anaphylaxis is relatively simple. Any of the following symptoms requires prompt injection of epinephrine:
- Any throat, lung, circulatory, or heart symptoms
- Two or more organ systems become affected (e.g., skin and gastrointestinal symptoms)
- Vomiting (recommended because it may be difficult to absorb oral antihistamines)
Once epinephrine is administered, an antihistamine should also be administered. If there are respiratory symptoms, albuterol can be administered as well.
If the allergic reaction is limited to isolated skin symptoms, oral symptoms or throat itching, or gastrointestinal symptoms not including vomiting, you can use an oral antihistamine first and observe the person very closely, with a source of epinephrine ready to be used if symptoms progress.
There is some debate about what to do for someone with a past history of a severe reaction who has eaten the food allergen or was suspected to have eaten the allergen but has not yet developed any symptoms of an allergic reaction. Some care plans strongly urge that epinephrine be immediately given or that an antihistamine should immediately be given. Some experts have advocated that this is the best strategy. Others have advocated treatment according to the symptoms that develop. It is difficult to say what the best strategy is. There is minimal downside to using epinephrine – it will “work” for mild symptoms and should not result in adverse reactions beyond some temporary local pain, bruising, and short-term jitteriness. It is unknown whether presumptive use of epinephrine contributes to reduced quality of life. Sit down with your doctor to discuss the pros and cons of what to do in these situations.
It is important to be deliberate and not hesitate when you have to use epinephrine. The device is potentially life-saving and has far more benefit than risk.
Should your child receive a dose of epinephrine, he or she requires 4-6 hours of medical observation in case the reaction escalates or a second (biphasic) reaction occurs. Additional medications may be needed (steroids, antihistamine, or additional doses of epinephrine).
When a person is experiencing symptoms of anaphylaxis, additional steps should include:
- Eliminate all risks of additional allergen exposure.
- Call 9-1-1 and/or seek medical attention immediately. Monitoring or additional medications may be required.
- Repeated doses of epinephrine may be necessary every 10 minutes if the symptoms are not going away.
- After epinephrine has been administered, have the person lay down with his or her legs raised, if possible, to help restore blood flow to vital organs (heart, lungs, brain).
- Administer secondary medications to help the patient breathe, such as an asthma inhaler; antihistamines to relieve itching and hives; and other medications as directed in the Allergy and Anaphylaxis Emergency Plan or as instructed by emergency medical personnel.
Delays in giving epinephrine can result in rapid decline and death within a short amount of time.
When treating anaphylaxis, epinephrine is the first-line of treatment! Antihistamines, inhalers, and other treatments all have a delayed onset of action and should only be used as secondary treatment. These medications cannot be depended on to reverse anaphylaxis because they will not restore low blood pressure or poor circulation. Antihistamines in this case become secondary agents, to be used only after epinephrine has been given. They are still important to give, but not instead of epinephrine.
Allergists recommend that all individuals at risk for anaphylaxis carry TWO epinephrine auto-injectable devices with them at all times AND an Allergy & Anaphylaxis Emergency Plan (AAP) signed by a board-certified allergist.
** You should take your epinephrine auto‑injectors everywhere you go, but they should be kept at room temperature (25°C, 77°F) until the marked expiration date, when they should be replaced. Your epinephrine auto-injector should not be refrigerated or exposed to extreme heat or light. Keep these temperature requirements in mind if you’re thinking of putting your auto‑injectors in your car’s glove compartment, for example.
Download FAACT's Poster for Epinephrine Auto-Injector Options.
Visit FAACT Resources for more information. Visit FAACT's Education Resource Center for FREE and downloadable resources.
Epinephrine
Epinephrine (ep·uh·NEPH·rin): A form of adrenaline – a hormone the human body creates naturally in response to stress. When injected, epinephrine works rapidly to constrict blood vessels, which helps increase blood pressure and keep blood flowing to vital organs. (Anaphylaxis can cause a severe and life-threatening drop in blood pressure.) It also relaxes airways to improve breathing, relieves cramping in the gastrointestinal tract, decreases swelling, and helps blocks itching and hives.
Epinephrine is the first medication that should be administered when treating anaphylaxis. Epinephrine reverses symptoms and allows time to seek additional care. Side effects from epinephrine may include rapid heart rate, jitteriness, weakness, paleness, and headache. Side effects are generally mild and go away within a few minutes.
Epinephrine is typically injected into the upper, outer thigh. Auto-injectors are designed to go through clothing, so a dose can be administered immediately. If an individual accidentally injects the device into a finger, hand, or other area of the body, seek medical treatment in an emergency room immediately. (Epinephrine constricts blood vessels – which, when administered correctly, restores blood pressure).
** You should take your epinephrine auto‑injectors everywhere you go, but they should be kept at room temperature (25°C, 77°F) until the marked expiration date, when they should be replaced. Your epinephrine auto-injector should not be refrigerated or exposed to extreme heat or light. Keep these temperature requirements in mind if you’re thinking of putting your auto‑injectors in your car’s glove compartment, for example.
Download FAACT's Poster for Epinephrine Auto-Injector Options and AAP Allergy & Anaphylaxis Emergency Plan.
Visit FAACT Resources for more information.
.jpg)

Navigating the Food Allergy Treatment Decision Process
Considering or deciding to pursue management of a food allergy is a major decision that may result in mixed emotions. Therefore, this informational handout aims to offer guidance on navigating the exploration process and psychological considerations associated with food allergy treatments.
Food Allergy Treatments Available
The cornerstone of management remains strict allergen avoidance and treatment of accidental ingestions with epinephrine. However, people are choosing to explore food allergy treatments in order to build tolerance that may protect against a reaction in case of accidental allergen exposure. These treatments are not cures, but aim to offer desensitization through carefully controlled ongoing allergen exposure. Additionally, there are risks and benefits with all treatments.
The following are food allergy treatments currently being offered or researched via clinical trials. (Refer to the American College of Allergy, Asthma and Immunology for more information)
- Oral Immunotherapy (OIT) - Ingestion of increasing amounts of allergen orally.
- OIT protocols using regular foodstuffs have been used for over a decade in private practice
- Multiple published approaches in both academic and private practice settings
- In 2020, FDA approved Palforzia: a 12% light roast, defatted peanut flour OIT product (4-17 years)
- Flour in a capsule, capsule not ingested.
- Uses FDA-approved good manufacturing practices (standardized doses).
- Epicutaneous Immunotherapy (EPIT) - application (not ingestion) of allergen via patch placed on the skin.
- Biologics including omalizumab and dupilumab are currently being investigated for their therapeutic use in food allergies. Results to date are promising, suggesting efficacy and tolerability.
Other Recent Publications
-
The Immune Tolerance Network IMPACT trial funded by the NIH involving ~150 children found that giving peanut OIT to highly peanut-allergic children ages 1-3 years safely desensitized most of them to peanut and induced remission of peanut allergy in 21% of participants. Maintenance was 6 peanuts (2g) for ~2.5 years. Remission defined as being able to eat 16 peanuts (5g) of peanut protein, without having an allergic reaction 6 months after completing immunotherapy. Lower levels of peanut-specific IgE at the start of the trial and being younger predicted whether a child would achieve remission. Nearly all participants had at least one dose-related reaction during treatment, most were mild to moderate in severity. 21 children received epinephrine for 35 moderate reactions.
Interpretation: Initiation of OIT before age 4 was associated with an increase in both desensitization and remission. Development of remission correlated with immunological biomarkers. There is window of opportunity at a young age for intervention to induce remission of peanut allergy.
Jones SM, et al; Immune Tolerance Network. Efficacy and safety of oral immunotherapy in children aged 1-3 years with peanut allergy (the Immune Tolerance Network IMPACT trial): a randomized placebo-controlled study. Lancet. 2022 Jan 22;399(10322):359-371.
-
The Peanut Allergy Burden Study (PABS) is a cross-sectional quantitative survey designed to determine the real-world experience of patients and caregivers with PA. The objective of the study was to understand the real-world utilization of PArelated healthcare resources and the impact of PA on productivity.
Conclusion: many healthcare resources were utilized by patients with PA and there was a loss of productivity associated with PA for patients and caregivers.
McCann W, World Allergy Organ J. 2021 Mar 26;14(3):100525.
-
Open-label follow-up of Palforzia: the benefit of daily administration of Palforzia has been established in clinical trials, but limited data past the first year of treatment are available. This longitudinal analysis aimed to explore the impact of continued Palforzia maintenance dosing (300 mg/day) on efficacy, safety/tolerability, and food allergy-related quality of life.
Conclusion: daily treatment with Palforzia beyond 1 year leads to an improved safety/tolerability profile and continued clinical and immunological response.
Fernandez-Rivas M, Allergy. 2021 Jul 28.
Consider the Following When Exploring Food Allergy Treatments
• Explore Motivations: Explore your and your child’s motivations for undergoing treatment. While the reasons may differ, it’s important to continually assess everyone’s motivation throughout treatment, as they may change and impact commitment levels.
• Determine Commitment: Assess your and your child’s level of commitment, as this may help determine if treatment is a good fit, and even when to begin treatment. All food allergy therapies require significant commitment.
• Assess Anxiety or Fear: Assess anxiety prior to starting treatment. While experiencing anxiety and worry is normal before and during treatment, excessive anxiety prior to the onset may be a factor in deciding when to begin a treatment.
• Evaluate Confidence in Provider: Ask questions that will help determine your level of comfort and confidence in the board-certified allergist administering the treatment.
Evaluation Process Before Beginning Treatment
Before enrolling in a food allergy treatment, it’s important to gather enough information to help not only make the decision whether or not to pursue it, but also to evaluate the board-certified allergist providing the treatment. Below is a question guide to help navigate this evaluation process.
Treatment & Provider Information:
• What are the goals, expected outcomes, and specific protocols for treatment?
• Are oral food challenges required to confirm the allergy before starting treatment?
• Are oral food challenges required to determine effectiveness of the trearment?
• What is the follow-up or maintenance protocol after treatment?
• What is required of you/your child (i.e. appointment frequency, daily protocols)?
• Will treatment impact school, work, activities, or daily routines, and if so, how?
• How are viruses or illnesses navigated while taking part in the treatment?
• How does the provider address treatment-related anxiety that may arise?
• How familiar is the provider with the treatment?
Potential Benefits & Risks of Treatment:
• What are the potential risks and benefits of the treatment, medical or otherwise?
• Are anaphylactic reactions a potential risk of treatment?
• What are potential treatment setbacks, their likelihood, and how they are handled?
Office Procedures:
• Will appointments be with the provider, or associates within the practice?
• Is a provider on call 24 hours/day in case of emergencies?
Develop A Flexible Food Allergy Treatment Mindset
Experiencing rigid thoughts and actions is natural when faced with uncertainty, discomfort, and distress. However, flexibility, or the ability to adapt, is beneficial when navigating treatments.
The following tips can help establish a flexible mindset and approach to food allergy treatments:
• Establish open communication with your board-certified allergist and treatment team.
• Engage in shared decision-making to develop treatment timeline and goals.
• Understand that treatment is a process rather than just a desired outcome.
• Prepare for the possibility of setbacks, the need to alter approaches, or stop treatment
• Monitor anxiety levels, reaching out for counseling or support services if excessive.
Download FAACT's Navigating the Food Allergy Treatment Decision Process poster here.

Access to Healthcare Resources
NeedyMeds.org is a powerful resource and is a one-stop shop to find medication discounts, clinics, health care related programs and assistance by state and you can even find scholarships! The most efficient way to tackle this information-rich website is to click on the Getting Started tab and choose the Welcome New Users link. Once you are familiar with Needymeds.org, heading right over to Patient Savings brings you directly to finding discounts, affordable clinics, and even help filling out patient assistance forms.
Here are a few highlights which can be found at Needymeds.org:
- Save on Prescriptions – search by company, drug name, generic, brand or download a discount card
- Find help on filling out patient assistance program forms
- Discover local, free, and low-cost sliding scale clinics
- Find programs who assist with medical transportation costs
- View government healthcare programs
- Connect with retreats, camps, and recreational programs
- Learn how to become a Needy Meds advocate to help your community
.jpg)
FAACT's FIST to THIGH "SIGN"
What would you do if you needed epinephrine...but you couldn't be heard?
Do you have a "SIGN"?
There might be a time when you are too far away for someone to hear you clearly or anaphylaxis is making it difficult to speak.
Here is a "SIGN" you can use...
- Move in motion
- FIST to THIGH
- Wait a second
- Repeat again
- FIST to THIGH
Share this "SIGN" with others so they can quickly respond in an emergency.
And, please share this video to help FAACT spread the word about this potentially life-saving "SIGN"!
.jpg)
FAACT's FIST to THIGH "SIGN"
What would you do if you needed epinephrine...but you couldn't be heard?
Do you have a "SIGN"?
There might be a time when you are too far away for someone to hear you clearly or anaphylaxis is making it difficult to speak.
Here is a "SIGN" you can use...
- Move in motion
- FIST to THIGH
- Wait a second
- Repeat again
- FIST to THIGH
Share this "SIGN" with others so they can quickly respond in an emergency.
And, please share this video to help FAACT spread the word about this potentially life-saving "SIGN"!
.jpg)
Emergency Kit Contents
There are several medications that can be used to treat anaphylaxis. These include epinephrine, H1 antihistamines, H2 antihistamines, albuterol, and steroids. We recommend your emergency kit include the following:
-
Epinephrine: Epinephrine is the single most important drug in the anaphylaxis emergency kit. It will rapidly act to reverse any and all signs of anaphylaxis, but most importantly low blood pressure, poor heart rate, poor circulation, swelling, and asthma/bronchoconstriction. Epinephrine will also reverse skin and gastrointestinal symptoms.
-
H1 Antihistamines (e.g., Benadryl®): These medications block the effects of histamine released from the mast cell during an allergic reaction. This class of medication is particularly effective for skin symptoms and swelling that is not affecting the airways. This class of medication is not a good first choice for fainting, loss of consciousness, lethargy, difficulty breathing, low blood pressure, or poor circulation, but it can act as an important supporting medication to epinephrine.
-
H2 Antihistamine (e.g., Zantac®, Pepcid®, Tagamet®): These medications also block the effects of histamine but have a different target than their cousin, Benadryl. H2 antihistamines are particularly effective as a supporting medication, in particular when there are suspected cardiovascular symptoms, because they block the effects of histamine on the coronary arteries. They will also reduce abdominal discomfort from the histamine-triggered release of stomach acid.
-
Albuterol (if you have asthma): Albuterol rapidly reverses muscle constriction in the lungs that may contribute to wheezing, coughing, or shortness of breath. This should be administered right after epinephrine if respiratory symptoms are present.
A note on steroids in treating anaphylaxis: If you have gone to the emergency room for treatment of anaphylaxis, you likely have been given steroids. Steroids are very powerful anti-inflammatory drugs. However, steroids have little role in the acute management of anaphylaxis. It takes steroids up to 4-6 hours to begin working and therefore won’t help in the immediate treatment of anaphylaxis. However, they are important in preventing biphasic reactions as well as skin and respiratory symptoms. Steroids are often prescribed for up to three days after an anaphylactic reaction.
Visit FAACT Resources for more information.
.jpg)