Education
For School Personnel
Back to Category View
Field Trips for School Personnel
Field trip coordinators, chaperones/adults, and bus drivers should be prepared to deal with food allergies and respond to a student who may experience an anaphylactic reaction while travelling to and from school-related activities and on field trips. This pertains to students who have known allergies as well as students who may experience anaphylaxis for the first time without a history of allergic reactions.
A designated individual directly available to students with food allergies during school-sponsored events and on field trips should fully understand students’ food allergies and be confident in caring for these students, including recognizing the signs and symptoms of an allergic reaction, understanding students’ emergency action care plans, and knowing how to enact emergency procedures.
In planning for field trips, care should be taken to ensure a healthy and safe environment for all students, including students with food allergies. For example, a class should not visit a ranch where peanuts are fed to animals if a student has peanut allergy, and a class should avoid visiting an ice cream shop if students have a milk allergy. This does not mean that students with food allergies should be left behind. Trips should be planned that are inclusive of all students.
FAACTs
- There is no cure for food allergies. Strict avoidance of the food(s) is the only way to prevent a food allergy reaction from occurring.
- Every food allergy reaction has the possibility of developing into a life-threatening and potentially fatal allergic reaction.
Review FAACT's Best Practices for Field Trips to assist in the planning for food allergies on field trips. You may also visit FAACT’s Education Resource Center for additional tools and resources. A list of suggested downloads are located at the bottom of this page.
FAACT and MenuTrinfo® Partner on Food Service Training
For the millions of students living with food allergies, eating at the school cafeteria is not merely a convenience, it’s a gamble – with potentially fatal consequences. The food service industry’s food allergy expert, MenuTrinfo®, partnered with the nation’s leading food allergy education and advocacy group, the Food Allergy & Anaphylaxis Connection Team (FAACT), to make serving students with food allergies safer.
Together, FAACT and MenuTrinfo® are providing leading-edge food allergy education, risk-reduction strategies, and emergency preparedness plans to food service facilities so they can safely serve students living with food allergies as well as their families, friends, and colleagues.
The AllerTrain™ suite of courses by MenuTrinfo® was launched in 2011 to meet the growing need for food-allergy and gluten-free training within the food service industry. Over the past decade, it has evolved into a wide variety of training options, led by the food service industry experts, designed to suit the needs of every member of the food service industry. The ground-breaking partnership with FAACT brings expert oversight and additional content vetted by FAACT’s Medical Advisory Board to achieve even stronger and clearer education for those who complete the training.
With both an eLearning platform and live workshops taught by Master Trainers, AllerTrain™ is an accessible option for every style of learner. MenuTrinfo® is the only company that offers an in-person food allergy training option, which is the chosen teaching to have students retain high levels of information.
AllerTrain U™ for the college and university settings and AllerTrain Lite™ are the programs that dining services looking to be “Certified Free-From” locations have turned to for the knowledge their staff must have to deliver food services with confidence each and every time. Both are ANAB/ANSI-accredited training courses that go further to meet state- and county-specific training mandates. You can find a map online showing college and universities that have utilized the AllerTrain™, AllerTrain U™, and AllerTrain Lite™ training.
The courses teach food service professionals:
- Top foods that cause allergic reactions
- Proper protocol for preparing food to avoid cross-contact with allergens
- How to better serve students with special dietary needs
- Recommendations for policy implementation
- Information on current and pending legislation in each state
AllerTrain™ and FAACT are helping food service professionals on all levels to better handle gluten-free and food allergen requests, avoid food allergy-related incidents, and prepare for onsite food allergy emergencies should they occur.
Has your college/university food service division provided certified allergen training for staff? If not, please consider using the AllerTrain™ U and/or AllerTrain™ programs to train all food service personnel. It’s the best way to ensure the safety of your students living with food allergies.
MenuTrinfo® also offers the Kitchens With Confidence™ program, which certifies food service locations that have been assessed through rigorous audits on methods, standards, policies, and understanding to serve persons with special dietary needs, specifically food allergies. A map of certified locations available on the AllerTrain™ website is a useful tool for students going to college with food allergies.
Visit AllerTrain™ to schedule your training today!

Best Practices for Coordinators and Designated Chaperones/Adults Include:
- Students with food allergies should participate in all school activities and must not be excluded based on their condition.
- Students should wear medical alert identification at all times.
- Encourage, but do not require, parents/guardians of food-allergic students to accompany their child on school trips.
- When planning for a field trip, the parents, school nurse, and field trip coordinators should collaborate to avoid high-risk destinations.
- If a trip includes an overnight stay at a hotel, request rooms with kitchens, refrigerators, and microwaves so food-allergic students can cook their own meals.
- Call all destination locations, including travel stops, restaurants, and hotels, ahead of time to ensure accommodations are available for student(s) with food allergies. Review emergency protocols with appropriate representatives from each of these locations.
- If a trip includes eating lunch outside at a park or picnic area, determine an alternate location in advance in the event of inclement weather.
- Designate the appropriate individual to work with the school nurse immediately prior to the trip to ensure all medications and instructions are packed.
- Identify for students and chaperones/other staff the trained individual(s) or the designated staff member(s) who will be carrying the student’s auto-injectors and other medications.
- Consider insect sting, medication, and latex allergies in addition to food allergies.
- Enforce a “No Food or Beverage Sharing” policy.
- Ensure backup batteries for cell phones and other emergency communication devices are available and in working order. Plan emergency procedures for areas in which cell phone reception may not be available.
- Enforce rules to wash hands before and after drinking/eating when possible (and use of disposable wipes otherwise).
- Participate in the school’s approach on how to manage students with food allergies.
- Understand how to directly communicate with the student’s parent(s) in the event of an emergency and ensure all designated adults have emergency contact numbers.
- Understand federal and state laws that protect the privacy and confidentiality of the student’s medical information and other legal rights of students with food allergies.
- How to report food allergy bullying or complaints from the student.
- Ensuring communication devices are in working order prior to each transport.
- Return all medication(s) to designated staff member or school nurse immediately upon returning from field trip.
Prepare for snack needs on long-haul trips:
- Notify all parents to avoid packing snack items that directly contain allergens.
- Require that snack/food items containing allergens remain wrapped until students are at their destination.
- Prepare allergy friendly snacks for all students and distribute them enroute. Consult with the school nurse and parent(s) of food-allergic students on approved snack items before to the trip.
- Provide disposable wipes to all students after eating snacks/meals.
Ensure you understand the role of the transportation staff while on field trips:
- Where the emergency action care plan is kept for each student
- Location of epinephrine auto-injectors and other emergency medication and how to administer it for each student.
Creating a safe environment for food-allergic students:
- FAACT's Cross-Contact section: Cleaning procedures
- Enforcing a "No Food or Beverages" policy (exception for children with a medical condition).
- Student placement on the bus (while limiting potential for social isolation).
FAACT Posters
Prepare To Act
It is important that bus drivers and other transportation personnel prepare for and understand how to respond to a food allergy emergency.
Steps to take include:
- Ensure all bus drivers, bus attendants, and substitutes receive annual food allergy and anaphylaxis training.
- Learn how to recognize the signs and symptoms of an allergic reaction and anaphylaxis.
- Learn how to use all epinephrine auto-injector devices.
- Participate in semi-annual emergency drills.
- Act quickly; note student could be exposed prior to bus trip.
- Learn protocols and procedures for activating EMS.
- If an allergic reaction takes place, know the plan of action.
- Who is going to give epinephrine?
- Who is going to call 911 and by what method?
- Who is going to contact the parents? Where can these emergency numbers be located?
- Who is going to ride with the student to the hospital?
- Who is going to comfort and explain the situation to students on the bus and their parents
- Provide emergency communication device for each transport (cell phone, two-way radio, intercom, etc.), and require testing of the communication device prior to each transport.
- Does your route’s first responder carry epinephrine?
- Create and enforce policies that prohibit discrimination and bullying against all students, including those with food allergies.
- Create and maintain a bullying report procedure for students with life-threatening food allergies that allows the student to report bullying to school personnel and/or the Transportation Director.
- Create and maintain a policy for review after an emergency that includes the school administrators, school nurse, transportation staff, bus drivers, parents, EMS responders, staff members involved, the student, etc.
Investigate and Review
If an allergic reaction does take place on the school bus or while students are being transported in other ways, transportation personnel should:
- Attend the review meetings with parents, staff, and students.
- Review updates to the student’s Allergy & Anaphylaxis Emergency Plan and notify staff, aids, and substitute teachers.
- Confirm replacement of all emergency medications for the student(s).
Download FAACT's Bus Drivers and Transportation Personnel Handout.
Download FAACT's Bus Drivers and Transportation Personnel Checklist.

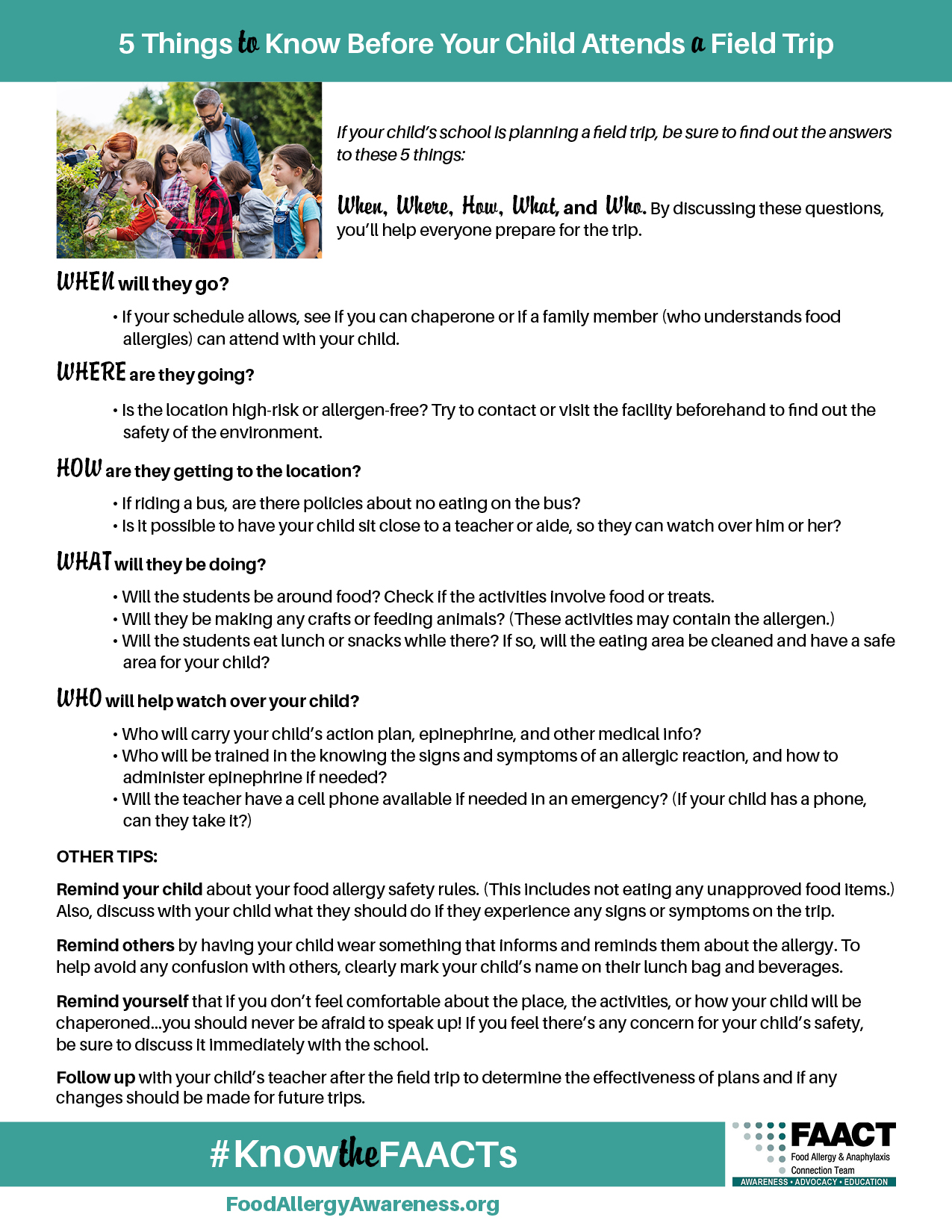
5 Things to Know Before Your Child Attends a Field Trip
If your child’s school is planning a field trip, be sure to find out the answers to these 5 things:
When, Where, How, What, and Who. By discussing these questions, you’ll help everyone prepare for the trip.
WHEN will they go?
- If your schedule allows, see if you can chaperone or if a family member (who understands food allergies) can attend with your child.
WHERE are they going?
- Is the location high-risk or allergen-free? Try to contact or visit the facility beforehand to find out the safety of the environment.
HOW are they getting to the location?
- If riding a bus, are there policies about no eating on the bus?
- Is it possible to have your child sit close to a teacher or aide, so they can watch over him or her?
WHAT will they be doing?
- Will the students be around food? Check if the activities involve food or treats.
- Will they be making any crafts or feeding animals? (These activities may contain the allergen.)
- Will the students eat lunch or snacks while there? If so, will the eating area be cleaned and have a safe area for your child?
WHO will help watch over your child?
- Who will carry your child’s action plan, epinephrine and other medical info?
- Who will be trained in the knowing the signs and symptoms of an allergic reaction, and how to administer epinephrine if needed?
- Will the teacher have a cell phone available if needed in an emergency? (If your child has a phone, can they take it?)
OTHER TIPS:
Remind your child about your food allergy safety rules. (This includes not eating any unapproved food items.) Also, discuss with your child what they should do if they experience any signs or symptoms on the trip.
Remind others by having your child wear something that informs and reminds them about the allergy. To help avoid any confusion with others, clearly mark your child’s name on their lunch bag and beverages.
Remind yourself that if you don’t feel comfortable about the place, the activities, or how your child will be chaperoned…you should never be afraid to speak up! If you feel there’s any concern for your child’s safety, be sure to discuss it immediately with the school.
Follow up with your child’s teacher after the field trip to determine the effectiveness of plans and if any changes should be made for future trips.
Download FAACT's 5 Things to Know Before Your Child Attends a Field Trip handout.
Additional Planning for Middle and High School
- Meet with parents individually to plan for each student’s needs while traveling.
- Have a plan for “check-in” among chaperones, coordinators, and students (when applicable) at designated times and immediately after snacks/meals. (Ensure a designated/trained individual meets with the group during meal and snack times.)
- Plan a group meeting with the student’s “buddy” (when using the “buddy system”) before the trip to review signs and symptoms of an allergic reaction and emergency procedures. Allow the student to share this information at his or her discretion – and if age appropriate – with an adult/parent/school nurse present.
When traveling by air, boat, or train, prepare in advance:
- Carry extra auto-injectors in their original packaging as backup.
- Ensure all names and prescription labels are attached to their original packaging.
- Keep liquid medication in the original containers, unopened.
- Keep a signed emergency action care plan and/or letter from the student’s doctor confirming the need for medication.
- Call ahead to speak with the concierge for cruises ships, airlines, and hotels to discuss dining alternatives to buffets and meals, as necessary; discuss meal planning during the student’s stay.
- Students should carry restaurant cards and notify a manager of their allergy upon arrival.
Prepare for emergencies:
- Locate health food and other allergy-friendly stores in the area.
- Locate pharmacies and hospitals.
- Carry and pack extra auto-injectors.
- Confirm travel arrangements in the event of an emergency.
- Carry doctor and other emergency contact numbers.
Resources and Downloads
- FAACT's Field Trips: Best Practices
- FAACT's Traveling with Food Allergies
- Food Allergy Safety: It's A Matter of FAACT!
- Food Allergy Management & Education (FAME) Toolkit
- Cleaning Methods
- Signs and Symptoms of Anaphylaxis
- More about Epinephrine
FAACTs
- Approximately 20 percent of cases requiring epinephrine administration in the school setting occurred outside the school building on the playground, traveling to and from the school, or on field trips.1
- Approximately 80 percent of severe allergic reactions requiring epinephrine among preschool children were left untreated. Factors resulting in under-treatment included lack of recognition of severity, epinephrine being unavailable, and fears about epinephrine administration.2
- 25 percent of first-time anaphylactic reactions reported in the school setting were those of students with no known history of an allergy.3,4
What is Anaphylaxis?
Anaphylaxis (an–a–fi–LAK–sis) is a serious allergic reaction that often involves swelling, hives, lowered blood pressure, and, in severe cases, shock. If anaphylactic shock isn\\'t treated immediately, it can be fatal.
References:
1 Pediatrics. 2005 Nov;116 (5):1134-40., Administration of epinephrine for life-threatening allergic reactions in school settings., McIntyre CL, Sheetz AH, Carroll CR, Young MC.
2 American Academy of Pediatrics, Allergic Reactions to Foods in Preschool-Aged Children in a Prospective Observational Food Allergy Study, David M. Fleischer, MD, Tamara T. Perry, MD, and Scott H. Sicherer, MD.
3 Sicherer SH, Furlong TJ, DeSimone J, Sampson HA. The US Peanut and Tree Nut Allergy Registry: characteristics of reactions in schools and day care. J Pediatr. 2001;138(4):560–565
4 McIntyre CL, Sheetz AH, Carroll CR, Young MC. Administration of epinephrine for life-threatening allergic reactions in school settings. Pediatrics. 2005;116(5):1134–1140
.jpg)
For School Personnel
With the increased number of students with food allergies now enrolled in schools – and 30 percent of food-allergic children allergic to multiple foods – increased education and resources for school personnel are essential.
True food allergies (as opposed to food intolerances) have the potential to become life-threatening. All school staff who interact with food-allergic students should understand the importance of food allergy management and the seriousness in food allergy reactions.
FAACT
Every food allergy reaction has the possibility of developing into a life-threatening and potentially fatal anaphylactic reaction.
.jpg)
For School Personnel
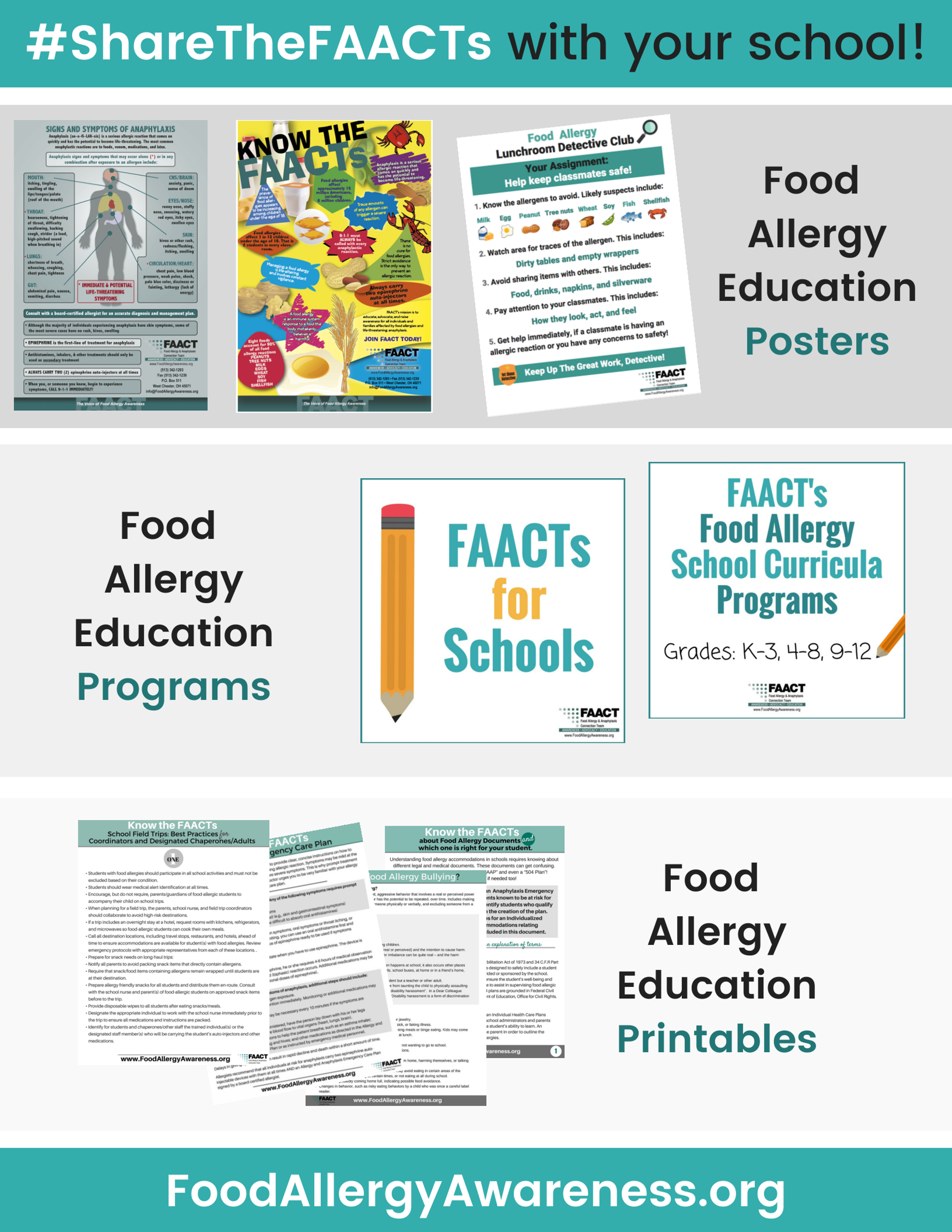
Helpful links and resources for School Personnel:
- FAACT's Food Allergy Curricula Program for Schools
- 'FAACTs for Schools' Program
- FAACT's School Lunchroom Poster
- FAACT's Education Resource Center
- FAACT's School Accommodations
- FAACT's Food Allergy School Letter to Parents (Sample Template)
- Food Allergy Management & Education (FAME) Toolkit
- School Access to Emergency Epinephrine Act
- The Need for Stock Epinephrine Auto-Injectors and Comprehensive Food Allergy and Anaphylaxis Management Plans in Schools, an Article Review
- National & Statewide School Guidelines
- AAP's Allergy & Anaphylaxis Emergency Plan
- Food Allergy Basics
- Food Allergy Safety - It's A Matter of FAACT!
- Anaphylaxis
- Signs & Symptoms
- Treatment & Management
- Food Allergens
- Food Labels
- Psychological Impacts
- Food Allergy Bullying Article with FAACT CEO, Eleanor Garrow-Holding, and Living Without Magazine, January 2013
Bus Drivers and Transportation Personnel
Food allergy is a growing safety and public health concern in the United States. Schools and transportation staff continue to face challenges each year due to the increasing number of students with food allergies. Bus drivers and transportation personnel are an important part of food allergy management plans and may have specific responsibilities under a student’s accommodation plan.
When school staff, physicians, parents, and other adults who interact with students join forces, it helps to create comprehensive management plans for students. Thorough details and guidance outlined in management plans will help to support the efforts of all those involved in caring for food-allergic students and will help make the school setting a safer environment.
FAACTs
- There is no cure for food allergies. Strict avoidance of the food(s) is the only way to prevent a food allergy reaction from occurring.
- Every food allergy reaction has the possibility of developing into a life-threatening and potentially fatal allergic reaction.
.jpg)
Guidelines for Food Service Personnel in Schools
With the increased number of students with food allergies now enrolled in schools – and 30 percent of food-allergic children allergic to multiple foods – increased education and resources for food service personnel are essential.
Mealtimes during school hours can be stressful for food-allergic students, their parents, school personnel, and food service personnel. The information provided here should be used to help create or strengthen food allergy management guidelines within food services in schools.
Accidents do happen, and all school personnel – including food service personnel – should be educated on emergency procedures should an allergic reaction occur. Food service personnel should attend all meetings prior to the beginning of the school year, and throughout the year as needed, regarding the needs of students with food allergies. This allows food service personnel the opportunity to learn about each student’s emergency action plan in addition to:
- Learning what foods each student must avoid.
- Learning best practices for the school year.
- Being able to ask questions about feeding the student.
- Being able to review the student’s Allergy and Anaphylaxis Emergency Plan.
- Receiving training on how to use prescribed auto-injector epinephrine devices.
- Learning about 504 accommodations or other plans in place for the students.
- Learning about student placement in the cafeteria and student safety and inclusion.
FAACT
There is no cure for food allergies. The only way to prevent a food allergy reaction from occurring is to avoid the offending food.
Download FAACT's Guidelines for Food Service Personnel in Schools: Best Practices & Prepare to Act.
.jpg)
Education for School Personnel
Educators are often the first to act in an emergency situation. Providing educators with the tools and information needed to care for food-allergic students will build the confidence needed to act quickly in an emergency.
Topics to cover in education for school personnel include basic food allergy medical facts, how to ensure students avoid allergens, the signs and symptoms of an allergic reaction, and how to enact emergency procedures. School policies and guidelines should include:
- Daily management of food allergies, allergen avoidance measures, emergency response, how to address bullying of and discrimination against students with food allergies.
- Strategic placement of medication, identifying the locations for school personnel and ensuring the medication is easily accessible and unlocked.
- Informing staff of all students who self-carry medications.
- Training school personnel in the administration of medications in accordance with governing laws.
- Working with the district’s transportation department on:
- Emergency procedures.
- “No food or beverage sharing” policies.
- Seat placement (while limiting potential for social isolation).
- Reporting harassment, bullying, or threats made against food-allergic students.
- Each student’s Allergy & Anaphylaxis Emergency Plan and other important information.
- Visit FAACT's Bus Drivers and Transportation Personnel section.
- Providing food allergy education for school personnel, students, parents, caretakers, and others who have contact with the student throughout the day.
- Identifying a core team to work with parents and the student to establish a prevention plan, including bus drivers, school counselors, teachers, substitute teachers, food service personnel, school administrators, the school nurse, and any other necessary individuals.
- Enforcing restrictions on permissible foods in the classroom and dedicated areas in the lunchroom.
- Arranging for emergency drills to include school personnel and first responders.
- Following applicable federal laws and identifying students with food allergies who qualify for Section 504 and other plans.
- State and federal laws that may apply to students with food allergies (e.g., stock epinephrine laws, self-carry medication laws).
- District policies and individual healthcare plans, 504 plans, etc., and procedures.
FAACT
Understanding how to enact emergency protocols in the event of an emergency ensures immediate action that could help save lives.
Download our free 'FAACTs for Schools' Staff Education Program.
The School’s Role
The school’s role in managing students with food allergies can seem daunting, especially for districts and schools currently that do not have a food allergy policy or guidelines in place.
At a minimum, FAACT recommends that schools require an Allergy & Anaphylaxis Emergency Plan (AAP) (signed by the student’s medical provider) for every food-allergic student and two auto-injectable epinephrine devices that are readily accessible, unlocked (or self-carried), and in a location known by every staff member in the school.
Each student’s emergency action care plan is like a guide on how to treat the student in the event of an emergency. It is signed by a doctor, giving the educator information on the student’s condition and specific instructions to follow should the signs and symptoms of an allergic reaction occur.
Partnering with parents and students will support efforts to improve the school setting for food-allergic students. Ask parents for guidance about the student – they are the experts on the child’s needs.
School staff should also carefully review the contents of this Web site and utilize the free downloads and resources available in FAACT's Education Resource Center to assist in caring for food-allergic students.
FAACTs
- In the school setting, when a school nurse or other licensed healthcare professional is not available to assist the student, the emergency action care plan should be as simple as possible.
- Allergy & Anaphylaxis Emergency Plan (AAP)
- A call to 9-1-1 and a trip to the emergency room should always follow epinephrine administration.
- Antihistamines alone should not be used to treat anaphylaxis. They can be administered after epinephrine. (See Treatment of Anaphylaxis for more details.)
- The signs and symptoms of an asthma attack and those of anaphylaxis can appear the same.Asthma medication (such as an albuterol inhaler) will only treat respiratory symptoms, while epinephrine will treat both an asthma symptoms and other symptoms of anaphylaxis.

Food Allergies on the Move
Students with food allergies can be particularly vulnerable on the bus traveling to and from school. Staff who are familiar with a student’s medical needs are absent. Due to the lack of direct adult supervision, students may be at a greater risk for exposure to food allergens, either intentionally or accidentally; bullying; and other factors that present a risk.
So it is important for school personnel, or other designated representative, to inform bus drivers and other transportation staff about students’ allergies and train transportation staff how to identify and respond to a student who may experience anaphylaxis. This pertains to students who have a known allergy as well as students who may experience anaphylaxis for the first time without a history of allergic reactions.
FAACTs
- In approximately 25 percent of epinephrine administration cases involving students and staff members, school personnel were not aware that the individual had a life-threatening allergy.2
- Approximately 20 percent of cases requiring epinephrine administration in the school setting occurred outside the school building on the playground, traveling to and from the school, or on field trips.2

Best Practices for Food Service Supervisors and Personnel
- Follow the guidance and utilize resources available from your local food service director, local board of heath, the U.S. Department of Agriculture (USDA), or registered dietitians trained in managing food allergies.
- Collaborate with your local food service director, the school staff and nurse, parents, and students’ physicians to share pertinent information about each student with food allergies prior to the start of each school year.
- Identify students with food allergies and become familiar with his or her allergy and anaphylaxis emergency care plan. School staff should keep the emergency care plan in a location that is easily accessible by food service personnel.
- Ask parents to provide you with a signed medical statement from the student’s physician outlining the management of the student’s allergens and avoidance measures.
- Know where each student’s emergency medications are stored (if they are not self-carried) and be trained in the administration of each student’s prescribed epinephrine auto-injector and any other necessary medications.
- Have a policy in place regarding label reading and keep a list of ingredients and product updates in appropriate and convenient areas, updating as necessary.
- Use separate utensils, pots, pans, cutting boards, etc., when preparing foods for food-allergic students. Learn how to effectively clean and store these items.
- Follow policies and guidelines to prevent allergic reactions and cross-contact from occurring.
- Learn about proper cleaning and removing allergens from surfaces and hands.
- Ensure food service staff clean all tables and chairs for use by students with food allergies.
- Attend all training and informational meetings on each student with a food allergy.
- Provide training to all cafeteria personnel on how to accommodate students with food allergies during mealtimes and when snacks are provided, including special events.
- Provide food service staff with resources to help assist in the management of students with food allergies.
- Implement and review cross-contact procedures. Visit FAACT’s Cross-Contact page for more information.
- Meet with parents upon request to review cafeteria menu items and ingredients and cafeteria procedures. This is especially important for students who are transitioning from half-day kindergarten to a full-day first grade or re-entry after an anaphylactic reaction at school.
- Display an ingredient label for each food on the cafeteria buffet line. This provides students the ability to self-educate as well as self-advocate.
Prepare To Act
It is important that food service personnel prepare for and understand how to respond to a food allergic emergency. Steps to take include:
- Annual food allergy and anaphylaxis training for all food service personnel.
- Learn the signs and symptoms of an allergic reaction.
- Learn how to use the student’s epinephrine auto-injector device and other medications.
- Advocate for emergency drills.
- Learn the procedure for activating EMS in an emergency.
- In the event of an emergency, follow the instructions provided by the physician on the student’s emergency action care plan.
- Additional concerns school staff need to prepare for in an emergency include:
- Who will give epinephrine? (Note the time the device was used – and write it on the device, if possible – for first responders).
- Who will call 9-1-1 and by what method?
- Who will retrieve the second epinephrine auto-injector and where will it be stored?
- Who will be outside the school to flag down first responders? (This is especially important in the private school setting or for schools located on large campuses.)
- Who will ride with the student to the hospital?
- Who will contact the parents?
- Where will the emergency numbers for the parents be located?
- Who will comfort remaining students and notify their parents (if needed)?
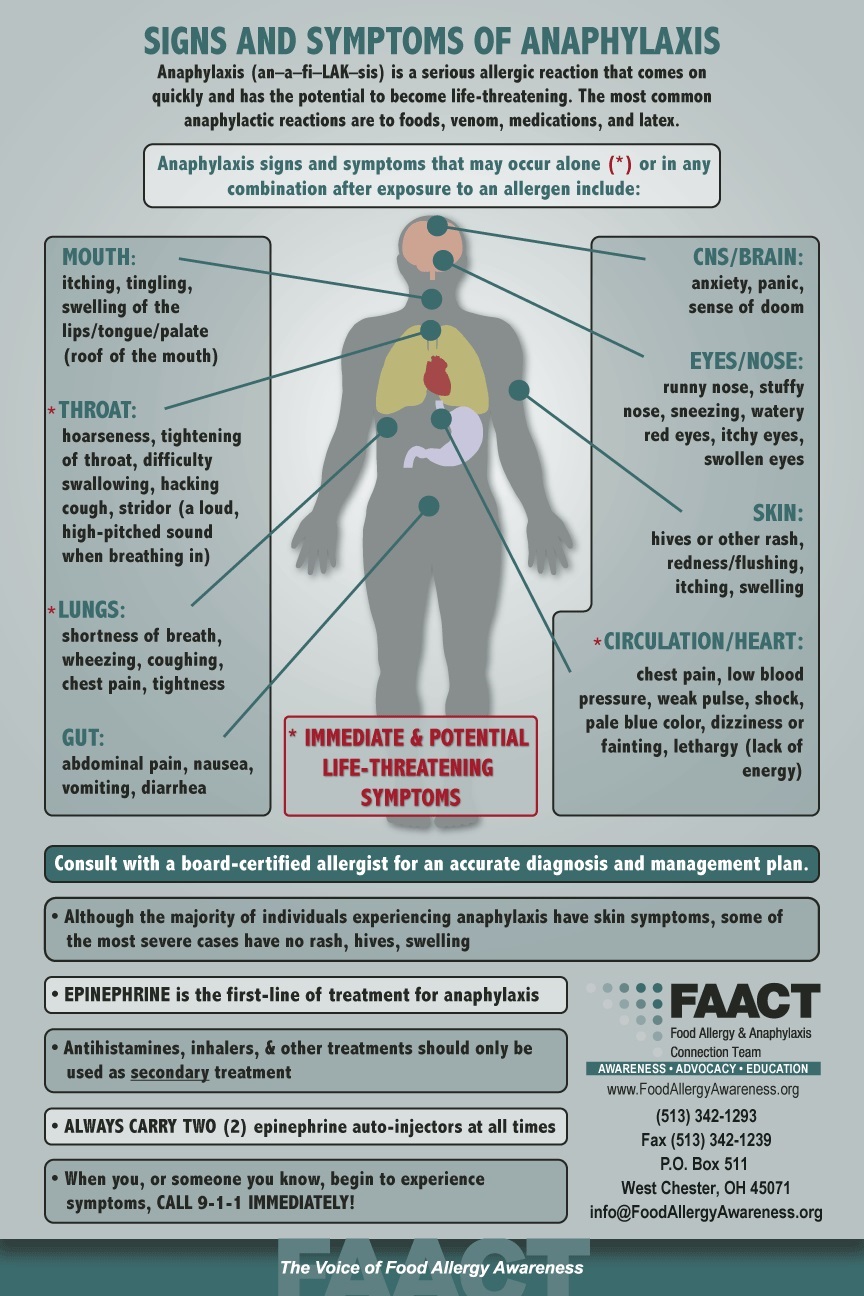
Signs & Symptoms
Signs and symptoms of an allergic reaction usually appear within a few minutes to several hours after exposure to a food allergen. If not treated promptly, food allergy reactions can be fatal. The student can also experience a second phase of their reaction called a biphasic reaction. This means the student may respond initially to treatment but experience symptoms later that are less severe, as severe, or even more severe than the initial reaction. After the administration of epinephrine, 9-1-1 should be called and students should always be transported to an emergency room for further treatment.
Understanding district policies and procedures on how to enact emergency protocol in the event of an emergency will help ensure swift action that can save lives.
Review the Bus Driver and Transportation Checklist to assist staff in planning for the management of students with life-threatening food allergies. You may also visit FAACT’s Education Resource Center for additional tools and resources, some of which are listed at the bottom of this page.
.jpg)
Resources for Food Service Personnel
- Food Allergy Basics
- Food Allergens
- Food Labels
- Food Service Personnel - Best Practices
- Cross-Contact (removing allergens)
- Food Allergy Management & Education (FAME) School Nutrition Toolkit
FAACT Posters
- 10 FAACTs to Know about Food Allergies
- Anaphylaxis Locations in Schools
- FAACT's Guidelines for Food Service Personnel in Schools: Best Practices & Prepare to Act
- FAACT's School Lunchroom Poster
- FAACT's School Programs for School Personnel
- Food Allergy Safety - It's A Matter of FAACT!
- Field Trips: Best Practices
- Newly Diagnosed with Food Allergies
- Preventing Cross-Contact
Visit FAACT’s Education Resource Center for additional tools and resources.
Resources for School Personnel
- FAACT's Food Allergy Curricula Program for Schools
- 'FAACTs for Schools' Program
- FAACT's School Lunchroom Poster
- FAACT's Food Allergy School Letter to Parents (Sample Template)
- CDC Voluntarily Guidelines or Managing Food Allergies in School
- Food Allergy Management & Education (FAME) Toolkit
- School Access to Emergency Epinephrine Act
- The Need for Stock Epinephrine Auto-Injectors and Comprehensive Food Allergy and Anaphylaxis Management Plans in Schools, an Article Review
School staff should carefully review the contents of this Web site and utilize the free downloads and resources available.
More information on food allergies in the school setting can be accessed in FAACT's Education Resource Center.
FAACT Posters
- 10 FAACTs about Food Allergies
- Allergy & Anaphylaxis Emergency Plan
- Anaphylaxis Locations in Schools
- Bullying - What Is Food Allergy Bullying?
- Bullying - Keys to Standing Up, Involvement, & Inclusion
- Bus Drivers & Transportation Personnel: Best Practices & Prepare to Act
- Bus Drivers & Transportation Personnel: Checklist
- Communicating with School Personnel: A Parents Guide
- FAACT's School Programs for School Personnel
- Field Trips - Best Practices
- Food Allergy Accommodations: Documents & Plans for School
- Food Allergy Education for School Personnel
- Food Allergy Safety - It's A Matter of FAACT!
- Food Service Personnel: Best Practices & Prepare to Act
- Newly Diagnosed with Food Allergies
- Preventing Cross-Contact
- Traveling with Food Allergies
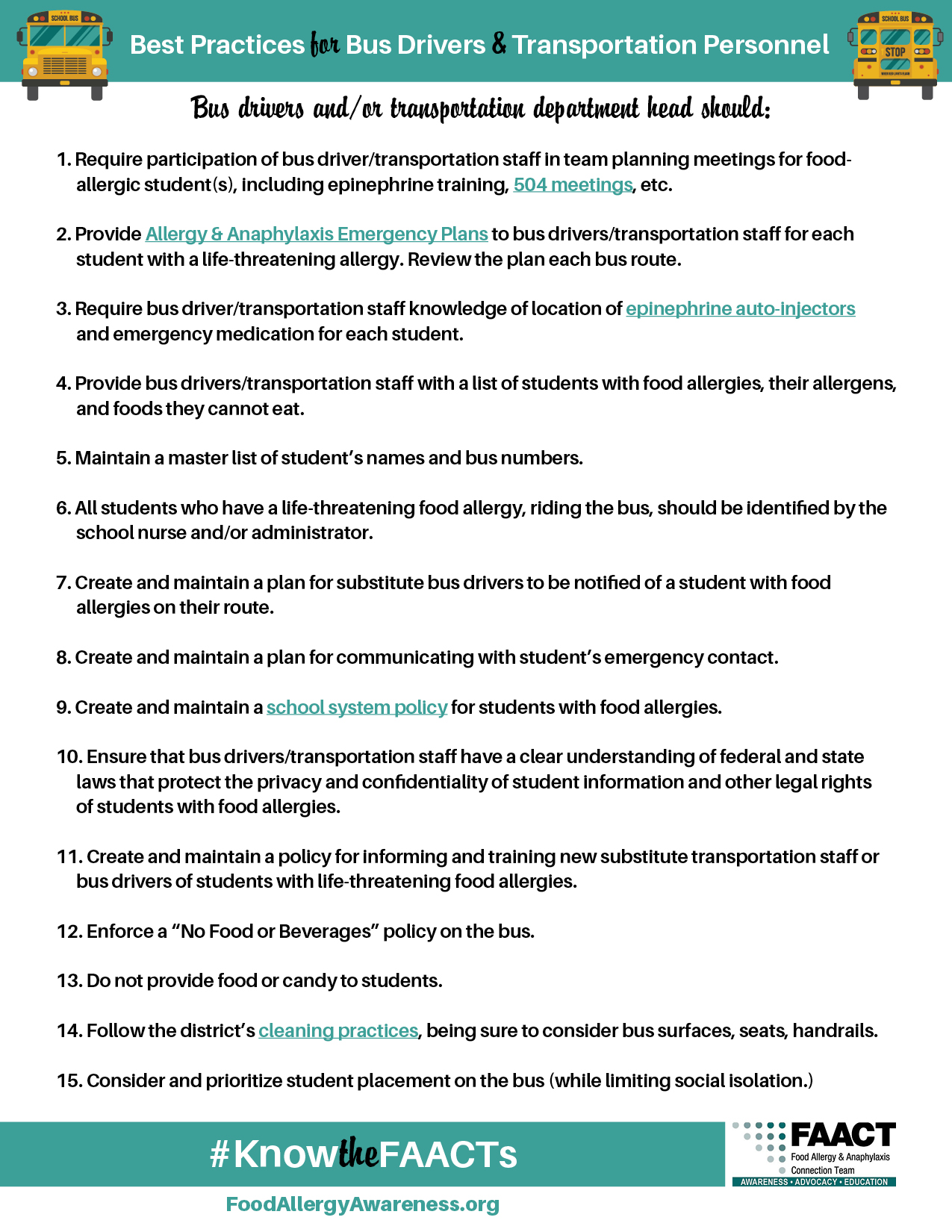
Best Practices for Bus Drivers and Transportation Personnel
Bus drivers and/or transportation department head should:
- Bus drivers and/or transportation department head should:Require participation of bus driver/transportation staff in staff food allergy and anaphylaxis training, including recognizing a reaction, administering epinephrine, etc.
- Encourage participation of bus driver/transportation staff in team planning meetings for food-allergic student(s). While it may not be practical for all transportation staff or bus drivers to attend all accommodation meetings, bus drivers and/or transportation staff will likely have responsibilities under a student’s 504 plan or other accommodation plan.
- Provide Allergy & Anaphylaxis Emergency Plans to bus drivers/transportation staff for each student with a life-threatening allergy. Review the plan each bus route.
- Require bus driver/transportation staff knowledge of location of epinephrine auto-injectors and emergency medication for each student.
- Provide bus drivers/transportation staff with a list of students with food allergies, their allergens, and foods they cannot eat.
- Maintain a master list of student’s names and bus numbers.
- All students who have a life-threatening food allergy, riding the bus, should be identified by the school nurse and/or administrator.
- Create and maintain a plan for substitute bus drivers to be notified of a student with food allergies on their route.
- Create and maintain a plan for communicating with student’s emergency contact.
- Create and maintain a school system policy for students with food allergies.
- Ensure that bus drivers/transportation staff have a clear understanding of federal and state laws that protect the privacy and confidentialities of student information and other legal rights of students with food allergies.
- Create and maintain a policy for informing and training new substitute transportation staff or bus drivers of students with life-threatening food allergies.
- Enforce a “No Food or Beverages” policy on the bus.
- Do not provide food or candy to students.
- Follow the district’s cleaning practices, being sure to consider bus surfaces, seats, handrails.
- Consider and prioritize student placement on the bus (while limiting social isolation).
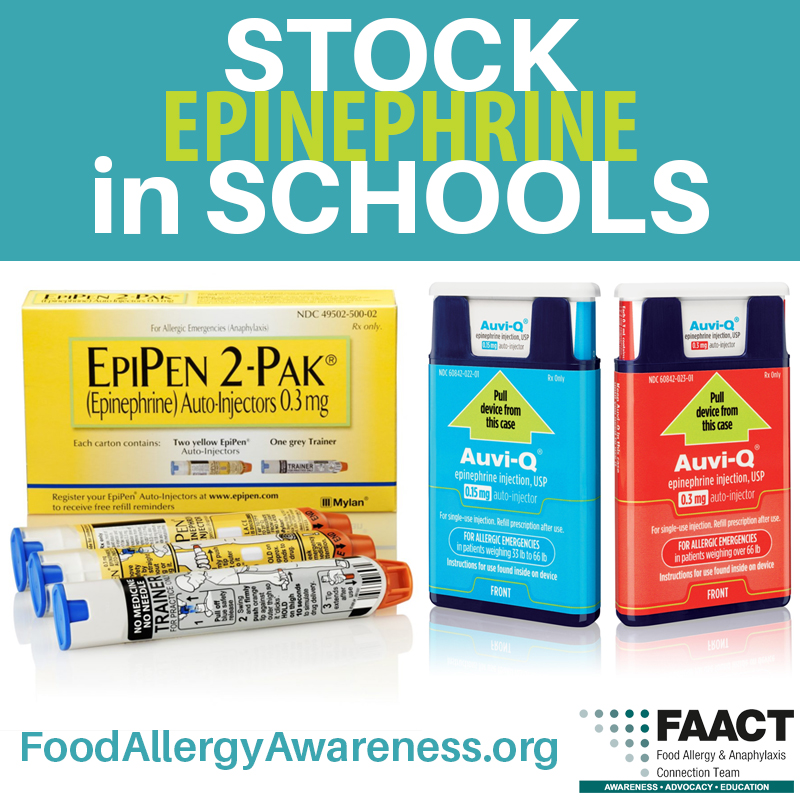
Stock Epinephrine in Schools
Many states have stock epinephrine laws in place that allow schools to keep a “stock” supply of epinephrine on schools grounds. Some laws allow for school staff trained in the administration of the medication to administer the medication to a student (and staff in some states) who appears to be in anaphylactic shock, whether the individual has a prescription or not.
In addition to protecting those who experience first-time anaphylaxis on school grounds, having the medication available also protects those who may require an additional dose of epinephrine or in case of a mechanical malfunction.
On November 13, 2013, President Obama signed into law the School Access to Emergency Epinephrine Act, which encourages states to adopt laws requiring schools to “stock” epinephrine auto-injectors. Financial incentives are provided for states mandating stock epinephrine in schools.
Learn more about stock epinephrine laws in your state by visiting the Government Relations section of FAACT’s website.
FAACTs
- 25 percent of first-time anaphylactic reactions reported in the school setting were those of students with no known history of an allergy.
- Studies report that 1 in 13 children in the United States have a food allergy. This averages to two children per classroom.
- In cases of fatalities from food allergy in the school setting, fatalities were associated with significant delays in administering epinephrine.
- 30 percent of children with food allergies are allergic to multiple foods.
- 1 out of 5 children with food allergies will have an allergic reaction while in school.
- Failure to properly recognize and a delay in treatment for anaphylaxis has led to fatalities in schools.
- Side effects of using epinephrine are usually mild and temporary
- In about one-third of anaphylactic reactions, a second round (or “phase”) of allergic reactions can occur after the initial anaphylactic reaction. This is called “biphasic anaphylaxis” A second reaction may happen as early as an hour after the first reaction or as long as 72 hours later (the average is 10 hours later) and can be less severe, as severe, or even more severe than the initial reaction.
- Every food allergy reaction has the possibility of developing into a life-threatening and potentially fatal reaction.
- There is no cure for food allergies. Avoidance is the only way to prevent a food allergy reaction from occurring.
- You cannot predict how severe a student’s reaction will be based on previous reactions. Students who previously had only “mild” reactions can later have dangerous and even life-threatening reactions.
- In approximately 20 percent of anaphylactic reactions, symptoms go away and will recur 1-3 hours later.
- More than 170 foods are known to cause a reaction in some people. However, eight foods account for 90 percent of all allergic reactions to foods:
- Milk
- Eggs
- Peanut
- Soy
- Wheat
- Tree nut (e.g., almonds, walnuts, pecans)
- Fish
- Shellfish (e.g., crab, lobster, shrimp)
Prepare To Act
It is important that bus drivers and other transportation personnel prepare for and understand how to respond to a food allergy emergency.
Steps to take include:
- Ensure all bus drivers, bus attendants, and substitutes receive annual food allergy and anaphylaxis training.
- Learn how to recognize the signs and symptoms of an allergic reaction and anaphylaxis.
- Learn how to use all epinephrine auto-injector devices.
- Participate in semi-annual emergency drills.
- Act quickly; note student could be exposed prior to bus trip.
- Learn protocols and procedures for activating EMS.
- If an allergic reaction takes place, know the plan of action.
- Who is going to give epinephrine?
- Who is going to call 911 and by what method?
- Who is going to contact the parents? Where can these emergency numbers be located?
- Who is going to ride with the student to the hospital?
- Who is going to comfort and explain the situation to students on the bus and their parents
- Provide emergency communication device for each transport (cell phone, two-way radio, intercom, etc.), and require testing of the communication device prior to each transport.
- Does your route’s first responder carry epinephrine?
- Create and enforce policies that prohibit discrimination and bullying against all students, including those with food allergies.
- Create and maintain a bullying report procedure for students with life-threatening food allergies that allows the student to report bullying to school personnel and/or the Transportation Director.
- Create and maintain a policy for review after an emergency that includes the school administrators, school nurse, transportation staff, bus drivers, parents, EMS responders, staff members involved, the student, etc.
Investigate and Review
If an allergic reaction does take place on the school bus or while students are being transported in other ways, transportation personnel should:
- Attend the review meetings with parents, staff, and students.
- Review updates to the student’s Allergy & Anaphylaxis Emergency Plan and notify staff, aids, and substitute teachers.
- Confirm replacement of all emergency medications for the student(s).
Download FAACT's Bus Drivers and Transportation Personnel Best Practices/Prepare to Act Handout.
Download FAACT's Bus Drivers and Transportation Personnel Checklist.
FAACT Posters
- 10 FAACTs to Know about Food Allergies
- Food Allergy Education for School Personnel
- Food Allergy Safety - It's A Matter of FAACT!
- Field Trips - Best Practices
- Preventing Cross-Contact
- Traveling with Food Allergies
Resources and Downloads
- Allery & Anaphylaxis Emergency Plan (AAP)
- Cleaning Methods
- Signs and Symptoms of Anaphylaxis
- More About Epinephrine
- Food Allergy Management & Education (FAME) Toolkit
FAACTs
- Teenagers and young adults with food allergies are at the highest risk of fatal, food-induced anaphylaxis.
- 25% of first-time allergic reactions reported in the school setting were those of students with no-known history of an allergy.
What is Anaphylaxis?
Anaphylaxis (an–a–fi–LAK–sis) is a serious allergic reaction that often involves swelling, hives, lowered blood pressure, and, in severe cases, shock. If anaphylactic shock isn’t treated immediately, it can be fatal.
References
2 “Administration of Epinephrine for Life-Threatening Allergic Reactions in School Settings.”
C. Lynne McIntyre, RN, PhD, Anne H. Sheetz, RN, MPH, Constance R. Carroll, RN, MPH, Michael C. Young, MD.
References
6.↵ McIntyre CL, Sheetz AH, Carroll CR, Young MC. Administration of epinephrine for life-threatening allergic reactions in school settings. Pediatrics. 2005;116(5):1134–1140
5.↵ Sicherer SH, Furlong TJ, DeSimone J, Sampson HA. The US Peanut and Tree Nut Allergy Registry: characteristics of reactions in schools and day care. J Pediatr. 2001;138(4):560–565
10.↵ Sampson HA, Mendelson LM, Rosen JP. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med. 1992;327(6):380–384
11.↵ Bock SA, Muñoz-Furlong A, Sampson HA. Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol. 2001;107(1):191–193
12. 2.↵ Bock SA, Muñoz-Furlong A, Sampson HA. Further fatalities caused by anaphylactic reactions to food, 2001–2006. J Allergy Clin Immunol. 2007;119(4):1016–1018
30.↵ Perry TT, Conover-Walker MK, Pomes A, Chapman MD, Wood RA. Distribution of peanut allergen in the environment. J Allergy Clin Immunol. 2004;113(5):973–976
2Management of food allergies in the school setting. Pediatrics. 2010; 126(6): 1232-1239. Sischer SH, Mahr T.