Blogs
Blogs
Entry Tags (354 found)
10-Years 8th-Graders AAAAI Action-Plan Action-plan Activities Adolescents Adults Advocacy advocacy Allergen-Free Allergies allergies Allergy allergy Allergy Management Allergy Safety Kit Allergy Travel Essentials Allergy-Awareness Allergy-awareness Allergy-Free Allergy-FreeRecipes Allergy-freerecipes Allergy-Friendly Allergy-Home Amusement-Parks Anaphylaxis Anaphylaxis-Action-Plan Anaphylaxis-action-plan APFED Asian-fare Asthma Awareness Back-To-School Back-to-school Baking bank Behavior Behavioral-Health Birthday Parties blog Blog Board-certified-allergist Bowls Bullying Busy Parents Camp Camp-tag Camp-TAG campaign Campaign CampTAG Camptag Canada Candy Caregivers Catered-events CDC Celebrations Celiac Celiac-Disease CEO Checklists Chicago Children Children with Allergies Christmas Civil-Rights civil-rights Civil-rights civilrights Civilrights Classroom Classroom Activities coalition Coalition College Community Compassion Contest CookbookAuthor cookbookauthor Cooking Coping Strategies Coronavirus Covid-19 COVID19 Dairy Dating DBV Technologies DBV-Technologies DEI Dining-Out Dining-out diningout Diningout Disaster-Preparedness Disasters Diversity Divvies Dorm Dorm Life early-intro Early-Intro Earthquake Easter Eating Education effort Egg EGID elementary Elementary Emergencies Emergency Emergency Plan Emotional Emotions Empathy EoE eosinophil Eosinophil Eosinophil-Awareness eosinophilicawareness eosinophilicawarnessweek epinephrine Epinephrine Equity FAACT FAACT Digital Influencer Summit FAACT-Teen-Conference Faact-teen-conference FAACT10Years FAACTs-Teal-Ghost FAACTs-TEAL-Heart FAAM FAAW Faaw FABConference FabConference Family FARRP Feelings Field-Trips Fish Floods food Food Food Allergies food-allergies Food-Allergies Food-Allergy Food-allergy Food-Allergy-Awarness-Month food-allergy-blog Food-allergy-blog Food-Bank Food-Industry Food-Manufacturer Food-Service FoodAllergyAwarenessWeek Foodallergyawarenessweek FoodAllergyBloggers-Conference Foodallergybloggers-conference FoodService foodservice Friends Friendship Giving Global Gluten Gluten-Free Graduation Grandparent Grateful Gratititude guidelines Guidelines Halloween Hanukkah Harvey Healthcare Heart High-School Holiday Holiday Traveling Holiday-Tips Holiday-tips Holidays Housing Hurricane ID Inclusion Industry Italy Juneteenth Know-The-FAACTs Know-the-faacts KyleDine Kyledine label Label Legacy Little-Northern-Bakehouse Manufacturer Martin Luther King Jr. Medic-alert Medic-Alert Medical Medical-alert-id Medical-Alert-ID Medical-id Medical-ID Medical-Singles Medication medications Medications Mental-Health Mental-Health-Awareness-Month Milk MLK Day MLK Jr. Mom Mother Mothers-Day MothersDay National-Peanut-Board Natural-Disasters NEAW Nima Nonprofit NPB Nurse Nurses nutfree-wok Nutfree-wok Nutrition Office Oral-Food-Challenge OWYN Parent Parent Guide Passover patient Patient Peanut peanut Peanut-Allergy Peanut-Butter pediatrician Pediatrician Picnic Pinterest Preparedness President Professional-Women Programs Psych PTSD Quarantine readlabels Readlabels Recipes Registered-Dietitians Registered-dietitians relief Research Residence-Hall Resilience Resources Restaurant Rights Risk Risk-taking Roommates Safety-Tips Safety-tips school School School-Lunch School-lunch School-nurse School-Nurse School-Resources School-resources secondary Secondary self-care Self-Care Self-care Senior Sesame Shellfish shelter Soy Spring Spring-Break Student Summer summer Summer-camp Summer-Camp Sunscreen Super-Bowl support Support Support-Group Support-group Teacher Teal Teal-Love Teal-Moments Teal-Pumpkin-Project Teal-Voices Teen-Conference Teen-conference Teen-Retreat TeenRetreat Teens Thank-You Thanksgiving Tia Mowry Time Saving Meal Prep Tips Top9 Tornados Traditional-Chinese-Medicine Traditional-chinese-medicine Traditions Transportation Travel Traveling Tree-Nuts TreeNuts Tweens UberEats United States University Vacation vacation Valentine Valentines-Day Valentines-day Vitality Vitality-Bowls Walmart WAO Welcome Wheat WHO Wildfires Work Workforce Workplace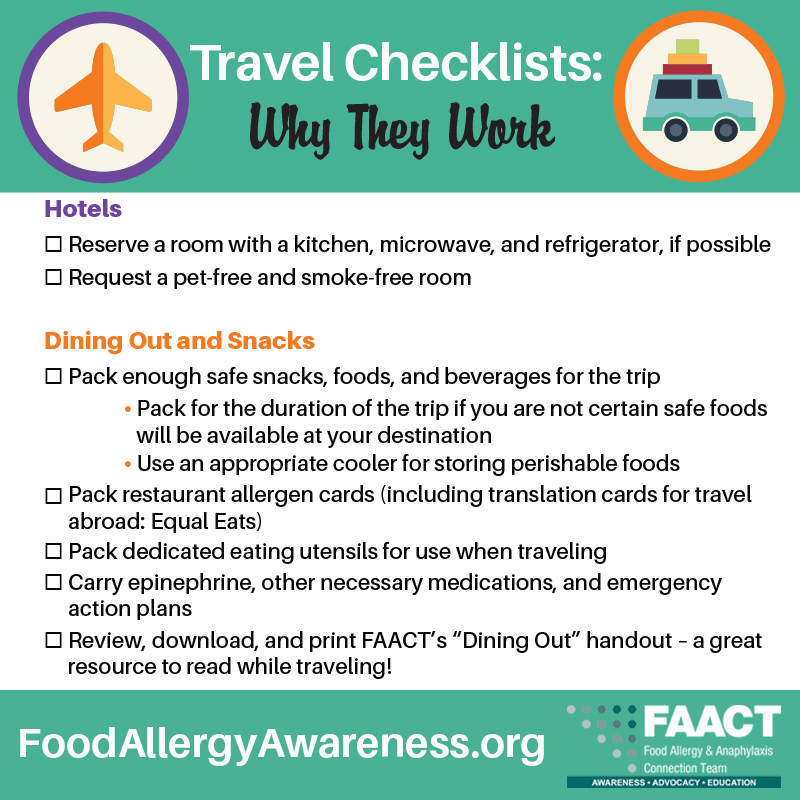
Travel Checklists: Why They Work
Travel Checklists: Why They Work
by Caroline Moassessi, FAACT Vice President of Community Relations
The last thing anyone needs when trying to plan a trip for a family managing food allergies is one...

Community Is at the Heart of Food Allergy Awareness
by Caroline Moassessi, FAACT Vice President of Community Relations
The bonds among our food allergy community run deep and strong. FAACT witnesses...

Admitted to College? Three Critical Steps to Take Now
by Caroline Moassessi, FAACT Vice President of Community Relations
Short on time but need to get organized about food allergies now that you sai...

Disaster Preparedness With Food Allergies: Lessons from the Recent California Fires
by Nicole Della Santina, MPH, FAACT Vice President of Public Health
The recent wildfires in southern California we...
Creative Ways To Celebrate Valentine's Day with Your Family
by Caroline Moassessi, FAACT Vice President of Community Relations
Family life is one of the most precious things we have. It is the heart...
Closing the Gap on K-12 Accommodations
Closing the Gap on K-12 Accommodations
by Caroline Moassessi, FAACT Vice President of Community Relations
Leaving your K-12 child in the care of a school district can be one of the most complex part...

Allergy-Safe Recipes for Busy Parents
As a parent, you’re no stranger to the demands of everyday life—between school drop-offs, extracurriculars, work schedules, and everything else that keeps your household running, your days are always ...
Holiday Guide for Parents with Allergic Children
The holidays are a time for joy, celebration, and making memories with family and friends. But as a parent of a child with food allergies, you may wonder how to balance all the excitement with the nee...

Tips for Traveling with Food Allergies
Are you feeling anxious about traveling with food allergies as the holiday season approaches? As we head into peak travel time, having a plan in place is more important than ever.
Navigating airports, ...

Making Holiday Memories With the Food Allergy Pivot
Whether you are celebrating Christmas, Hanukkah, Kwanzaa, or simply time off this winter, the season is perfect for creating cherished memories. Ho...

